 sai
sai
女性健康筛检:守护自己的健康
 sai
sai

 sai
sai
Dr Helena spoke on Breast Feeding’s benefit & myths on Living Delight Programme 8TV on 16/3/20. Click the link below to watch the full interview

Dr George Lee returns to discuss the latest medical news. Expect deep insights delivered with generous humour. Menopause is part and parcel of ageing for women, but the symptoms can be severe and the changes difficult to accept. But IVF specialists in Britain have proposed a new procedure that they say can delay menopause for up to 20 years. We’ll be speaking to Dr Helena Lim, consultant obstetrician and gynaecologist, to unpack this and whether delaying menopause is a possibility.


Dr Helena Spoke to First Classe Magazine about using contraception to control period : https://firstclasse.com.my/women-using-contraception-to-control-menstruation/

Dr Helena spoke to First Classe Magazine on Egg Freezing : https://firstclasse.com.my/egg-freezing-fertility-option/

The British Medical Journal published a new paper that said that fertility treatment facilities must be more transparent about the treatments offered. While this applies to the UK, what is the fertility treatment like in Malaysia? We speak to fertility specialist Dr Helena Lim who walks us through the whole process from start to end.





Recently, a large study of 1.8 million Danish women found that hormone contraceptives cause a small but significant increase in the risk for breast cancer. We speak to consultant obstetrician & gynaecologist Dr Helena Lim to find out if women should be alarmed.
http://www.bfm.my/dr-helena-lim-contraceptives-and-breast-cancer-risk.html
Your browser does not support native audio, but you can download this MP3 to listen on your device.

Period pain, a taboo topic that needs to be talked about. 80 percent of women have experienced menstrual cramps at some stage of their journey between puberty and menopause. Among them, 20 percent have pains severe enough to interfere with daily tasks and activities. Today, we have Dr Helena Lim, Consultant Obstetrician and Gynaecologist with us to bust myths about period pains and tell us how to survive through it all.
http://www.bfm.my/helena-lim-menstruation-survival-guide.html
Your browser does not support native audio, but you can download this MP3 to listen on your device.
 When it comes to family planning, women bear a disproportionate amount of the responsibility. There are very few male methods for family planning that are both practical and effective. Consultant obstetrician and gynaecologist Dr Helena Lim explores what’s on the horizon for safer and better family planning methods.
When it comes to family planning, women bear a disproportionate amount of the responsibility. There are very few male methods for family planning that are both practical and effective. Consultant obstetrician and gynaecologist Dr Helena Lim explores what’s on the horizon for safer and better family planning methods.
https://www.bfm.my/sharing-responsibility-for-family-planning
Your browser does not support native audio, but you can download this MP3 to listen on your device.



Question: I am current 40 years-old and would like to know what is my chance of getting pregnant with IVF. Can I choose the gender of my baby when I go through an IVF
Dr Helena’s Answer:
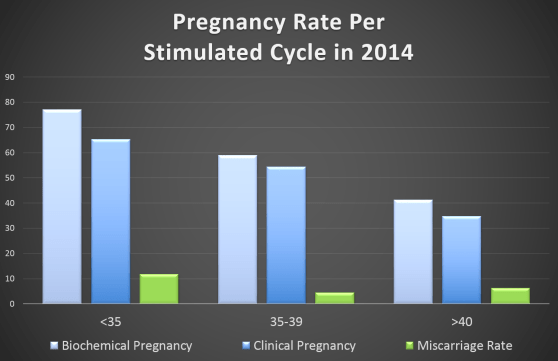
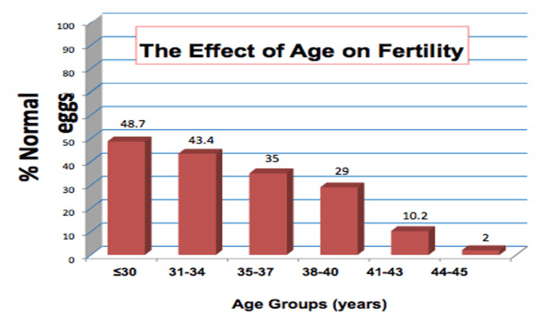
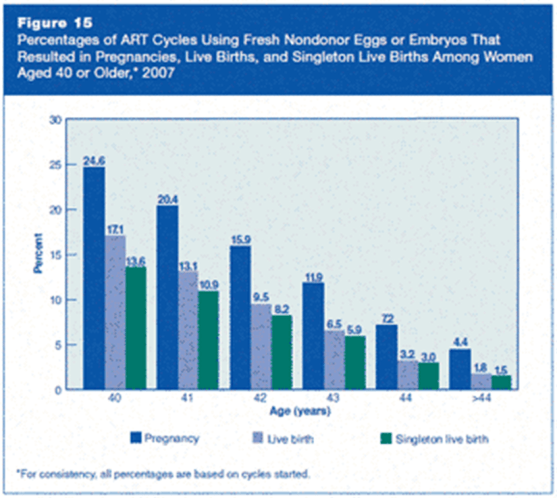
One of the biggest single determining factor for IVF success is the woman’s age. Before the age of 35, the IVF success rate is around 60-80%. After the age of 35, the success rate drops to 40-60%. The success rates of IVF drop drastically after the age of 40 to about 20-30% and then 1-2% after 45.
The reason for this is because as women aged, the number of follicles produce each menstrual cycle drop drastically. The quality of eggs also deteriorate as we age. As we aged, the division of chromosomes in our ovaries can become more imperfect, resulting production of eggs with faulty sets of chromosomes, leading to increase number of abnormal eggs and henceforth abnormal embryos.Therefore, women over the age of 40 has a lower rate of pregnancy with each individual IVF cycle, compare to their younger counterparts
This is a macroscopic view of the general population of women after the age of 40. However, an individual’s success rates is also dependent of her body condition, her ovarian reserves and her uterus receptivity. No two women at the age of 40 is exactly the same. A healthy 40 year-old woman with good ovarian reserves is more likely to produce good number of good quality embryos. Her counterpart who smokes and drinks, eats badly and have poor ovarian reserves is more likely to fail her IVF attempts.
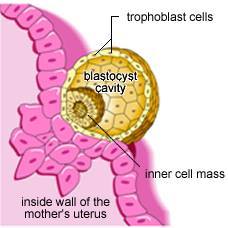
Recently, advances in Pre-implantation Screening (PGS) tests allowed us to biopsy embryos at blastocyst stage to select embryos which is normal in chromosomal make-up before embryo transfer. This test is extremely useful in determining which embryo is more likely to get our patients pregnant. However, like all the tests in this world, it comes with its problems as well. First and foremost, PGS is still expensive, and this test can only be done on embryos created from IVF, which then increase the cost of the IVF cycle. If the embryos tested showed that all the embryos are abnormal, there is no way we can change or treat these embryos and make them chromosomally normal. And therefore, some patients may end up not having any embryos which is suitable for transfer after an IVF with PGS. However, if this is the scenario, the couple can then move on quickly to another cycle of IVF to collect more embryos for PGS, hence, shortening the time required to find the ‘right’ embryo to achieve pregnancy.
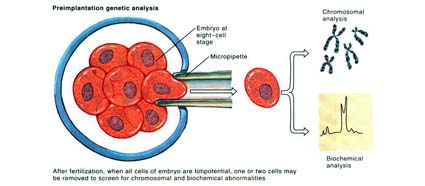
Although this technology is able to reveal the gender of the embryo, one must realize that the use of such technology to perform gender selection in STRICTLY Prohibited in this country and also most countries in this world. It is important to note that IVF and PGS are technologies to help couples to achieve a healthy pregnancy and must not be misuse for ones’ whims and fancies. Science and technology should be use sensibly to maintain and restore nature’s balances and any manipulation as such can potentially tip off the balance and create potential disasters to mankind.

Question: We are thinking of having an IVF but we are not sure which IVF Centres we should choose. Are all IVF Centres the same? What are the factors we should take into consideration?
Dr Helena’s Answer:
The world of Assisted Reproductive Medicine had evolved rapidly and the demand for reproductive services had increase by leaps and bounce as fertility rate in many countries had dropped dramatically. In Malaysia, the demand for fertility services had led to the establishment of many fertility centres.
However, are all fertility centres and fertility the same? What are the factors and issues we need to consider when choosing a fertility unit or a particular Doctor?
Here are some useful tips on how you choose your doctor and the fertility centre
(1) Does the fertility centre has good reputation for its success rates and quality control?
Unlike in other countries such as Australia or UK, in Malaysia, there is no compulsory reporting system for a fertility unit’s success rates and live birth rates. Therefore, it is extremely hard to get information about a particular Centre’s success rates. Some centres do publish their rates on their website, but again these rates are not verified by authorizing bodies and the way of calculation of success rates differs from one centre to another, making it very difficult to compare apple to apple. Therefore, it maybe worthwhile to check with people you know who had been through IVF at these centres, to gather more information about a particular centre
Due to a recent incidence of mixing-up patient’s gametes in one particular centre in Singapore, many countries such as Singapore had now made it mandatory to have international accreditations for the fertility centres in order to have license to operate. Although this has not been the case in Malaysia, a small number of reputable IVF centres had been granted international accreditation after going through robust auditing process. One of the example of this accreditation is called RTAC Certification. The Reproductive Technology Accreditation Committee (RTAC) is a subcommittee of the Board of the Fertility Society of Australia and reports directly to that Board. It is charged with the responsibility of setting standards for the performance of ART through an audited Code of Practice and the granting of licences to practice ART within Australia. It further licences an International Version of the Code of Practice for the use by Certifying Bodies in countries outside Australia and New Zealand. These are some important markers to ensure good quality control and would serve as one of the key deciding factors for patients when they choose a particular IVF centre.

(2) Does the fertility centre has qualified doctors and lab scientists?
Fertility doctors are mainly Gynaecologist with special interest and training in Fertility. The lab scientists are called embryologists and their training involved reproductive lab sciences. It maybe worthwhile checking the doctors and embryologists qualifications to ensure they have the appropriate training to handle your IVF.

(3) Does the team at the Fertility Centre make you feel comfortable?
Fertility journey can be a daunting experience and hence a professional team who makes you at ease is important to support you through this journey. A team who is genuinely concerned about your wellbeing, sincere about helping you in every step of your fertility journey is the backbone to your fertility success

(4) Did the doctor spend enough time assessing your fertility issues and personalized your treatment plan?
Many people has a misconception that IVF is a standard cookbook and the doctor/ fertility centre just need to follow the recipe to achieve a pregnancy. Whilst this conception is true to some extent when it involves standard operating procedures in IVF, however, there are areas with subtle differences which can make a whole lot of difference to the outcome of an IVF. Variation such as choices in types of protocols used in patients, dosage and types of medications, clinical monitoring, protocols in the fertility lab and decisions on the timing of embryos transfers are some of the examples. A good IVF Doctor would be able to critically analyze a couple’s fertility problem and personalize the treatment plan for individual needs

(5) Does the fertility centre has new technology which has been proven useful clinically?
IVF world is always full of excitement with advent of new technology everyday. As much as we would like to embrace all the new technologies by investing on new machines and lab equipment, which in turn would increase the cost of IVF for patients, one need to ask whether these new technologies are proven useful clinically. Therefore, it is important to find out whether the added tests/ technology on the standard IVF is indicated for your condition. It is important to discuss with your doctor the risk and benefit of the extra tests/ technologies before going through your IVF.
Question: We are thinking of going through an IVF, but we are concerned whether IVF babies have higher risk of abnormalities. We are also concerned that IVF babies are less healthy than their counter-parts and have shorter life-span, is it true?
Dr Helena’s answer:
Since the advent of IVF and Assisted Reproductive Technology, there had been constant debates on its safety and implication towards the health of the next generation. One of the biggest concerns is whether these fertility treatment will give rise to increase risk of congenital abnormalities in babies born as a result of IVF.
These debates and concerns are certainly valid. After all, the process of IVF in creating life outside human body in a Petri dish and then putting them back into the human body to let it grow into a baby is certainly mind blowing. How would we ensure that the doctors and scientists know what they are doing? And mind you, the IVF process were the results of many trials and errors. What makes you think the product (which is the baby), is not plagued with defects and errors?
Intensive research in the early years, and a thriving population that has now grown to more than 5 million IVF children worldwide, have reassured scientists, but they have not stopped studying and trying to improve the process.
Recent discoveries in epigenetics – the study of how environmental factors can affect gene activity, and how a person’s risk of getting chronic diseases is “programmed” into them before they are even born – have opened up new possibilities.
Much of today’s research stems from the Barker hypothesis, which proposes that birth weight may be linked to the likelihood of getting certain diseases. IVF babies are known to have lower average birth weights – even if the difference, at about 20-30 grams, is small. Scientists are now investigating whether IVF conception equates with more hospital admissions, and an increased risk of cardiovascular disease, high blood pressure and diabetes in later life. However, there is no good evidence as yet to suggest likewise
A recent study by the Human Fertilization and Embryology Authority, which linked 106, 381 HFEA register records from 1992-2008 to the UK’s National Registry of Childhood Tumours (NRCT) is one of the largest population-based linkage studies ever carried out. This study has found no association between ART and childhood cancer. This finding offers comfort to those patients facing the difficult decision about whether to undergo fertility treatment or not.
In 2012, scientists at the University of California, Los Angeles (UCLA) looked at birth defects among infants born both via IVF and conceived through natural means in California, which has the country’s highest rate of IVF use. They included babies born after IVF and other assisted reproductive treatments such as couples’ use of fertility-enhancing drugs and artificial insemination.
Among 4795 babies born after IVF and 46,025 infants who were conceived naturally, 3,463 babies had congenital birth defects. Even after controlling for factors that can affect such birth defects, such as mother’s age, and race, which can influence rates of genetic and environmentally driven developmental disorders, 9% of infants born after IVF had birth defects compared to 6.6% of babies who were conceived naturally. Overall, the babies born after IVF were 1.25 times more likely to be born with abnormalities. The researchers did not find a link between birth defects and other fertility treatments like artificial insemination or ovulation induction.
It’s possible that the higher rate of abnormalities with IVF is due in part to whatever was contributing to infertility in the first place, say the researchers. But some of the researchers’ view was the fact that an increase was not seen among babies conceived using artificial insemination or ovulation induction suggests that process of IVF itself, in which eggs are removed from a woman, fertilized in a dish with sperm and then allowed to develop into embryos, which are transplanted back into the womb, is the primary culprit.
However, another more recent study in 2016 by researchers from the University of Adelaide and the University of Melbourne. The study reviewed all assisted reproduction technologies carried out in South Australia over a 16-year period from 1986 to 2002.
This was linked to data on birth outcomes from the South Australian Birth Defects Register (SABDR). The register includes a record of all live births, stillbirths, terminations, birth weight and congenital defects. Birth defects were also followed up for five years. The researchers looked at the statistical link between maternal factors and birth defects, and compared this between babies either conceived naturally or by IVF and ICSI. The study found no statistically significant increase in birth defect. There was some suggestion by the press that this study suggest that IVF reduces the incidence of birth defect in women after the age of 40, but was refuted by the research group due to its misleading nature.
With the advent of Pre-implantation genetic screening (PGS) & Pre-implantation genetic diagnosis (PGD), which is fast gaining popularity, scientist can now screen embryos to exclude chromosomal and genetic abnormalities. The use of these technologies may further decrease the incidence of birth defect and congenital abnormalities associated with chromosomal defects or genetic issues. However, more long term data is required to support this hypotheses.
In conclusion, although there had been great hypothetical concerns about the risk of cancers & birth defects amongst babies born following Assisted Reproductive Technologies (ART), the actual link is difficult to establish due to many confounding factors such as parental age, the cause of infertility and etc. the actual incidence of childhood cancers and birth defects are small and should not be a great stumbling stone to those who are considering going through fertility treatment to have their babies
Question: My husband and I had gone through 3 IVFs without success, does it mean that our chance of pregnancy is very slim? Is it due to my body condition?
Dr Helena’s Answer: To achieve a successful pregnancy through IVF, there are some basic pre-requisite factors:
(1) The age of the couple, especially the female partner
(2) The duration of Subfertility
(3) good quality and quantity of eggs and sperms to make good quality embryos
(4) a conducive uterus environment for implantation
Studies had also shown that there is a increasing cumulative pregnancy rate for women who went through a few cycles of IVF.
However, after going through three IVF without success, one may wonder whether there is light at the end of the tunnel.
Being a fertility doctor, I can understand how frustrating it would be. However, these IVF cycles which did not work out, may contain valuable information about your fertility. As we know, apart from being a treatment in its own right, IVF also serve as a diagnostic tool in its own right, by telling us how you respond to the medications, how your eggs and sperms qualities are, and how your embryos qualities are.
There a a few aspects we may consider to improve on for your next IVF treatment:
The IVF treatment protocol
The clinic
The sperm
The eggs
The uterus
Here are some consideration for you:
(1) The IVF Treatment protocol.

While the IVF treatment protocol is pretty standard, every patient responds differently to the types and dosage of IVF medication. Each cycle teaches us how your body responds to the injections to help your follicles grow. It takes a good IVF doctor to be able to decide on the right dose and right type of medications, to get you to produce an optimal number of high quality eggs. Some young patients with normal ovarian reserve grow well in response to a standard protocol, patients with poor ovarian reserve and those with PCOS need a lot of extra attention and closer monitoring.
However, at the end of the day, some of this is trial and error. A good previous record can help us to learn from each cycle , until we can customize the perfect protocol for you
(2) The IVF clinic/centre.
It is important to note most IVF clinic/ centre are pretty standard, there are variations in terms of their operations and quality controls, and hence their success rates. In Malaysia, there is still no regulatory body that mandates each IVF clinic/ centre to report their success rates. However, it is important to look for credible centres with proper accreditation to ensure the quality of your IVF treatment.
(3) The sperm.

Poor sperm quantity & quality may be associated with failed fertilization of an egg during an IVF but with the advent of ICSI, these problems are easily over-come. However, if the sperms are have high DNA fragmentation, the resulting embryos may still have poor quality. Simple lifestyle changes such as stop smoking & alcohol, weight loose, exercise and consumption of good quality food which are rich in anti-oxidants are some of the key elements in improving sperm quality and IVF outcome
(4) The eggs.

Human egg is a thousand times bigger than the sperm, and that the energy for cell division during embryo cleavage comes from the mitochondria in the egg’s cytoplasm, therefore, egg quality is another important factor for IVF success. Poor egg quality leads to poor embryos and hence failed IVF. The problem is that it’s very hard to make this diagnosis, as there is no blood tests or medical technology to identify poor eggs prior to an IVF cycle. In fact, IVF is a diagnostic tool in it own right, as egg quality can be assess during an IVF. To improve egg quality involves making lifestyle changes, improving diets, and sometimes some alternative medications such as DHEA.
(5) The uterus.

It is probably a very Oriental or ‘Chinese’ believe that failure to get pregnant/ implantation is always the fault of the uterus. It is not unusually to hear the terminology of ‘cold uterus’ being cited for the reason for not getting pregnant. Hence, the idea of surrogacy has become very popular recently because of the disproportionate amount of media attention it attracts, and especially so when cross borders IVF had become extremely popular with the ease of medical access overseas. This had lead to the idea that the best medical solution for them after many failed IVF cycles is surrogacy. After all, the fact that the embryos are not implanting means the uterus must be ” defective” , so doesn’t it make sense to use a fertile woman’s uterus as an incubator for 9 months ? However, the truth is that surrogacy is an expensive and complex treatment option, which is best reserved for women without a uterus. It is also important to stress that Surrogacy is ILLEGAL in Malaysia. Research shows that the reason for failed implantation is much more likely to be genetically abnormal embryos ( because of poor quality sperms or eggs), rather than a uterine problem. However, in about 20-30% of women, failure in implantation maybe due to some small correctable issues in the uterus such as polyps or fibroids. These issues can be dealt with easily without having to resort to surrogacy

However, if you have no embryos frozen, what is your option?
This chart below showed a cumulative live IVF births from a study conducted.
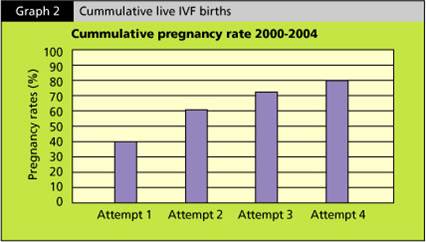
This study looked at all the women under the age of 42, who are going through IVF.
The study revealed that the pregnancy rate is around 40% in this group of women after they completed their first cycle of IVF. For those women who did not get pregnant the first round and went on having the second round of IVF, there were another 20% who got pregnant after the second round. Therefore, by the 4th IVF cycle, around 80% of women would have achieved a live birth.
This statistic clearly shows that if you persevere and keep moving on, chances of you getting pregnant by the end of the 4th IVF is around 80%.

Therefore, it is not unusual for Fertility doctors to encourage our patients to keep moving on because the statistics had clearly show us the evidence.
To improve your chance of pregnancy for the next IVF, it is important to improve the quality of your eggs and sperms by eating healthy and improve lifestyle, quit habits which can potentially jeopardize your success rates such as smoking, alcohol and stress. Speak to your fertility doctor about what are the other options in your IVF treatment.


Question: I am a person who is fearful of pain. I gathered that going through IVF will required multiple injections, surgery and other procedures which are painful. Is it true?
Dr Helena’s answer:
IVF sounds daunting to many people. A lot of us have perceptions that it is extremely expensive. Some of us thinks that it would bring us a lot of inconvenience, such as having to go to hospital everyday, lay in bed for a few months, quit our job and etc
One of the greatest fear many had was the perception of pain associated with IVF procedures. The thought of having daily injections made most of us wanting to run away and hide from the doctors. Some people are scared thinking about the egg retrieval procedures. Some are dreading the embryo transfer procedure, thinking that it would bring great pain and discomfort. Some dread the injections which are taken after the procedure, which are the progestogen injections, aimed to support the lining of the uterus whilst the embryos are implanting.
However, with the new development and breakthroughs in the world of reproductive medicine, IVF procedures had become more and more comfortable and easy to management, with minimal disruption to daily life.
First and foremost, the durations of injections had been shortened significantly with the use of antagonist injections in IVF. This method of doing IVF is called the antagonist cycle or the short protocol. So, instead of having 3 weeks of injections in the agonist cycle or long protocol, the advent of antagonist injections had lead to a shortened period of 10-12 days of injections. This had greatly reduce the discomfort one needs to go through with injections.
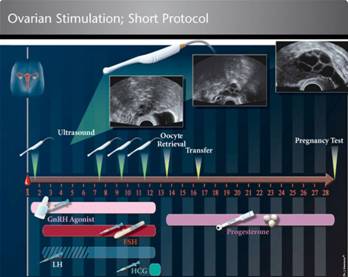
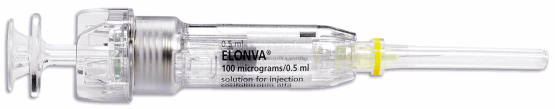
The use of self-administered FSH injection pens with extremely fine needles, had significantly cut down the pain one experienced during injections. This self- administered injections pens are given to patients to take home, and the injections are administered by patients themselves, so patients do not need to come to the clinic or hospital to have their daily injections. The needles used are similar to the ones used in the insulin injection pens, which is extremely fine and almost painless.

There is also another long acting FSH injection which given at the beginning of an IVF cycle and can last for 7 days. After the initial injection, the patient need not take FSH injection for the next 7 days, which significantly cuts down the number of injections required.
The egg retrieval procedure which usually happened after 10-12 days of injections involved having a light sedation in an operating theatre. In the past, the use of certain sedations such as Valium, Dormicum or pethidine administered by the IVF doctors whilst performing the egg retrieval procedure had appeared to be increasingly unsafe. In many IVF units, a proper IVF operating theatre with a trained Anaesthetist giving sedation during the egg retrieval procedure is becoming a norm and deemed acceptable in terms of safety. One of the advantage of the involvement of an Anaesthetist is that egg retrieval procedure is becoming almost painless, and hence optimizing patient experience in IVF.

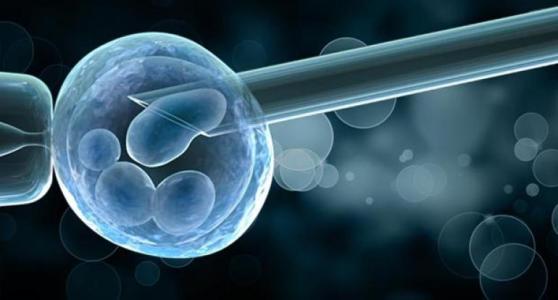
Embryo transfer procedure is usually carried out 3-5 days after the egg retrieval. During the procedure, the embryos which were created following fertilization of the retrieved eggs with sperms are replaced into the uterus. This procedure is performed without anaesthesia or sedation, is relatively pain free. The experience is almost the same as having a cervical smear. Therefore, women should not feel fearful about having an embryo transfer.

After the embryo transfer, to support the uterus lining and to ease implantation, a
Progestogen is prescribed. In the past, progestogen is administered by injections. These injections are usually painful and cause local irritations, which is uncomfortable and unacceptable to many. With the advent of effective oral and vaginal suppository preparations, studies had shown that these forms of progestogen are equally effective in delivering progestogen to uterus, injectable progestogen had slowly becoming a thing of the past in many IVF centres. This has also greatly cut down the pain experience in IVF
In conclusion, with rapid modernization in reproductive medicine & technology, IVF had become relatively painless. It is importantly to find out more information on IVF before you embark on this journey.


Question: My Husband & I had been married for 8 years, we have tried many different methods of getting pregnancy with no avail (except IVF). The reason I have not attempted IVF is because I heard that it is extremely expensive with low success rates, is this true?
Dr Helena’s Answer: Many people have a lot of myths and misunderstanding about IVF. In fact, IVF started in the 1970’s with many controversies. It used to be regarded as cultic practice in science, intertwined with many religious, social and ethical controversies
However, many years had gone by and IVF had progressed in leaps and bounds in its technology and approach, proving to the world its value and safety. At the turn of this century, reproductive doctors and scientists had achieved many new innovations and breakthroughs, to make IVF more accessible and safer. Hence, IVF had gradually become the mainstream in reproductive science, making the dreams of having children a reality for many couples
However, it is not unusual to find that people are still weary about IVF, and there are still myths and misconceptions surrounding IVF.
One of the myths about IVF is that it’s extremely costly. We hear stories that people had to ‘loose an arm or a leg’ to be able to afford IVF.
The truth is that IVF cost had reduced remarkably for the last 10-20 years, thanks to many creative innovations, especially in the advent of cost effective medications, culture mediums and lab equipments. The advent of a new freezing technique, called vitrification, allows IVF scientists to freeze embryos more effectively to allow storage of excessive embryos, to be used later, cutting down the need to repeat another IVF cycle, making IVF more cost effective.
The cost of IVF in Malaysia is generally ranging between RM12,000-RM20,000. The price range varies because of differences in clinical and laboratory settings, medications used and etc
The success rates are generally good depending on the age of the women. For women aged below 35, the success rate is about 60-80%. For women above the age of 35 but below the age of 40, the success rate is around 50%. The success rate fell dramatically after the women crossed 40 years of age.
There is recent study on Danish population about the cost effectiveness of IVF. The study followed almost 20,000 Danish women undergoing fertility treatments including IVF. Within three years, 65% of the women had given birth, with the figure rising to 71% within five years.
Therefore, it is important to find out more about IVF before deciding on or against it.

Can IVF Cause Cancer?
Today’s post addresses a question that I am often asked at the clinic – Can IVF cause cancer?
This concern very likely stems from a study done 12 years ago, which has since been well-publicised. It reported that the use of Clomid, which is a fertility medication widely used to treat ovulatory dysfunction in women, might increase the risk of breast and uterine cancer.
Understandably, this has caused some infertility patients to wonder if the treatments they will undergo are safe. Therefore, today I’d like to reassure you by providing references to other studies on the subject.
It’s important to note that since that study was first published, more studies have been conducted and most have found no significant link between Clomid use and cancer risk. One such study, which in fact offers the strongest evidence that Clomid and other ovarian-stimulating drugs do not increase the risk of ovarian cancer, comes from the Cochrane Review.
Published in 2013, the review looked at studies from 1990 to February 2013 that involved 182,972 women. The review not only found no evidence of increased ovarian cancer in women who use any fertility drug, but also pointed out that studies claiming there is an increased cancer risk were unreliable. This is because their sample sizes were too small for drawing conclusions and they did not take into consideration other potential risks for cancer.
For example, if a woman has never experienced pregnancy, her risk of cancer increases. Certain causes of infertility can also cause an increased risk of cancer, for example obesity, PCOS and endometriosis. So in fact, the increased risk of cancer noted in those studies may not be related to the medications at all.
In fact, ironically, some studies showed a decreased risk of developing breast and uterine cancer among infertile women on Clomid, in comparison to infertile women who did not seek treatment for infertility.
There are two other studies, with substantial sample sizes, which included 25,108 women from the Netherlands who received IVF treatment between 1980 and 1995, found that there was no increased risk of breast cancer. Another study, by the Institute of Child Health at University College London, which involved over 250,000 British women undergoing IVF between 1991 and 2010, also found no increased risk of breast or uterine cancer in those patients. However, they learned that IVF patients had a slightly higher risk of ovarian cancer – 15 in 10,000 odds, as compared to women who had never undergone IVF, who had 11 in 10,000 odds.
So as a consensus, from the studies quoted above and others like them, you can rest assured that fertility drugs like Clomid do not increase your risk of developing breast or uterine cancer. However, because infertility itself is a cancer risk factor, it is best that you undergo the necessary follow-up after your infertility diagnosis.
Should you have any concerns on the medications and treatments for infertility, please don’t hesitate to speak to your infertility consultant.


Endometrial scratching to improve IVF success rates
Couples who are struggling with infertility often seek In-Vitro Fertilisation (IVF) treatment in order to improve their chances of starting a family. But what happens when you have gone through multiple unsuccessful IVF cycles? Is there something else you can try?
Many patients who’ve experienced this first hand, have asked me this question, eager to try out something new to enhance their chances in the next IVF cycle. Therefore, today, I’d like to tell you more about a procedure called endometrial scratching, which has become increasingly popular in recent years.
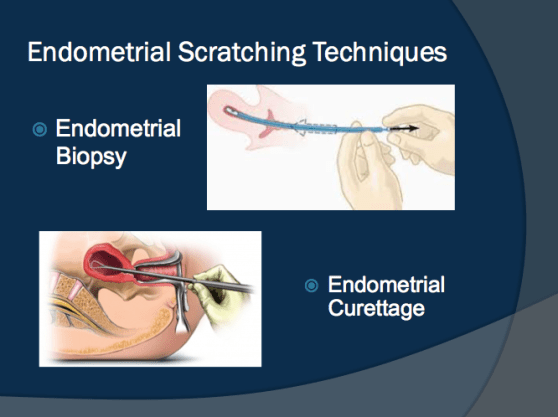
What is it?
Endometrial scratching is a procedure that involves agitation of the endometrium, which is the mucus membrane that lines the uterus. For conception to occur, a fertilised egg has to successfully implant itself into the wall of the uterus. Sometimes, implantation fails, usually due to the quality of the embryo or the receptivity of the endometrium. In endometrial scratching, a fertility specialist passes a special thin catheter or pipille through a woman’s cervix. The pipille is then moved up and down to gently make tiny scratches or scrapes in the uterine lining. The similar effect can also be achieved by introducing a hysteroscope through the cervix to visualised the lining of the uterus during polyps removal.
Why is it done?
In theory, endometrial scratching is believed to trigger the uterus to repair itself and develop a new lining, which will be more receptive to an embryo implanting. While the effectiveness of the procedure needs further investigation, studies that have been done on endometrial scratching in recent years have shown encouraging results.
One such study was conducted by the University of Nottingham, UK, which involved 158 women who had undergone unsuccessful IVF procedures. The women were divided into two groups, with one group given the endometrial scratching procedure. As a result, they found the women who had undergone the scratching procedure achieved a 49% pregnancy rate, compared to 29% in the other group.
In another study involving 1000 women, presented at the annual meeting of European Society of Human Reproduction and Embryology (ESHRE), endometrial scratching is said to increase pregnancy success rates for couples trying to conceive naturally or with Intrauterine Insemination (IUI).
When is it done?
The endometrial scratching procedure is usually recommended for patients who’ve experienced multiple unsuccessful IVF cycles or Intracytoplasmic Sperm Injection (ICSI) treatment. The procedure is best performed prior to a woman’s period or right after the period. It is done before an IVF or frozen embryo transfer (FET) cycle begins.
Does it hurt?
While the endometrial scratching procedure has been described as generally painless, requiring no anaesthetic, some women do experience discomfort during and after the procedure. The pain is similar to period cramps and there may be slight bleeding afterwards. To help with possible discomfort, patients are advised to take over-the-counter pain medication about an hour before undergoing the scratching procedure.
If you’ve gone through several IVF attempts and are keen on learning more about endometrial scratching, take the next step and ask your fertility specialist if it is right for you.
What you should know about AMH
When you seek medical advice for infertility issues, one of the hormone tests that you be advice to take is the Anti-Mullerian Hormone or AMH test. This test measures the AMH levels in your blood, which helps doctors determine your ovarian or egg reserve.
In this post, I’ll explain what egg reserves and AMH tests are, as well as what you can do if your AMH levels are low:
About egg reserves
Humans are born with a limited amount of eggs. To be precise, a girl is born with between one to two million immature eggs or follicles in her ovaries. But not all these follicles will survive into adulthood. In fact, throughout a woman’s life, the majority of her immature eggs will die in a natural process called atresia.
Did you know that by the time a girl has her first period, only about 400,000 follicles are left? And with each subsequent period, she loses about a thousand follicles, while just one matures into an ovum or egg. This means, throughout her reproductive life, a woman will develop only about 400 ovum. The number of developing follicles a woman has left, is called her “ovarian or egg reserve.”
Egg reserves and the quality of those eggs vary from one woman to another, due to factors such as age and infertility. Over time, both the quantity and quality of a woman’s eggs gradually decreases. Therefore, when seeking treatment for infertility, it is important for a woman to gain insight into the remaining quantity of her egg reserve and fertile years.
What is AMH?
When follicles develop in a woman’s egg reserve, her body release the Anti-Müllerian Hormone (AMH). AMH levels, therefore, can give us a good idea of the state of a woman’s ovarian reserve. Since AMH levels are determined by the number of developing follicles in a woman’s ovaries, low AMH levels are an indication that the ovarian reserve is depleted.
Fewer developing follicles mean slimmer chances for a mature and healthy egg to be released and fertilised. As such, when a woman knows the state of her egg reserve, she can determine how urgently she requires treatment.
AMH testing
While egg reserves generally decline in the mid to late 30s, leading to low AMH, age is not the only factor. Environmental factors can also cause low AMH, such as cancer treatment and inherited genetic causes. AMH levels can be easily assessed with a blood test, but like most diagnostic tests, it has its limitations. For example, it cannot indicate the quality of the eggs that are left, which requires a separate test. However, as AMH levels remain fairly constant in a woman’s cycle, she can have the test at any time.
What Can’t AMH tells you
As much as we would like to believe that AMH is ‘the ultimate test’ for ovarian reserves, however, it only tells us some aspect of your fertility performances but not all. AMH does not tell you the quality of your eggs. Therefore, some women who have plenty of eggs and high AMH level may not perform well in an IVF treatment cycle because of poor egg quality.
For women who take oral contraceptive pills, AMH level may not be a true reflection of their ovarian reserves. Those who were taking the pill had 19 percent lower levels of AMH and 16 percent fewer early-stage follicles.
Recently, there has been clinical studies which reported that there is a significant variation in serum AMH levels across the menstrual cycle regardless of ovulatory status. This variability, although statistically significant, is not large enough to warrant a change in current clinical practice to time AMH measurements to cycle day/phase.
What you can do
If you should take an AMH test and find that your level is low, do not lose heart! Your AMH level is just one piece in a complex jigsaw puzzle. Your best course of action is to discuss matters with your infertility specialist. Ask your doctor how you can protect your egg count and health, as well as discuss the best possible solution to your problem. For example, DHEA supplementation and well-managed IVF protocols have been shown to be effective in improving IVF pregnancy rates in women with low AMH. Maintain a positive outlook and don’t give up on your dreams of having a baby!
Can IVF bring on early menopause?
One of the most common question patients like to ask about IVF is that whether the treatment itself will bring on Menopause earlier. This is probably by far one of the greatest myths about IVF which we would like to clarify.
A woman’s ovaries contain immature eggs sacs known as follicles, which have the potential of developing into mature eggs. However, most of these follicles will be lost without having fulfilled their purpose.
Women are born with millions of eggs in their ovaries. These eggs are quiescent in the ovaries until the women reach the age of menarche (when they get their first menses). At that time, the eggs in the ovaries started to come up after hibernating for 10-16 years. This is due to a pulsatile release of hormones from the organs below our brain called hypothalamus and pituitary. So, at the start of our menses, our ovaries will recruit around 10-20 eggs at one go. However, after the menses, our body will only choose one egg to grow. The rest of the eggs will regress and die off. With the help of our hormones, the particular ‘chosen’ egg with grow to a certain size and maturity, and then ovulation will occur. Hence, we only release one mature egg every menstrual cycle.
But of these many follicles, only one of them will become dominant and mature. The others that do not get a chance to mature and release an egg, will simply disintegrate and be lost in a natural process called atresia. The loss of these follicles during each menstrual cycle means that several undeveloped eggs are also lost.
Therefore, throughout a woman’s reproductive life, her ovaries will release only around 400 eggs, despite being born with millions of eggs. So basically, we ‘wasted’ around 12-20 each menstrual cycle, until the day when we reach menopause, whereby there is NO eggs in our ovaries
So if a woman can naturally produce only one egg per menstrual cycle? How do IVF specialists harvest several eggs at once?
For a woman who is undergoing an IVF treatment, the use of injectable fertility drugs (hormonal drugs) will stimulate her ovaries to overcome the natural tendency of choosing one dominant egg and ‘wasting’ other eggs produced during this particular cycle. In this scenario, the hormonal injections will stimulate all the eggs recruited during this particular cycle to grow simultaneously. Once these eggs reached a certain size and maturity, they are being harvested during an egg retrieval procedure
When a woman undergoes IVF, she will be prescribed with injections containing FSH. The amount given will be several times higher than what her body would naturally produce. This high amount of FSH will stimulate a lot more follicles than usual and help more of them to mature into eggs. An important thing to understand is that FSH will only act on the follicles that a woman’s body will naturally produce each month. Therefore, there is no depletion of the overall egg supply. And when those eggs are harvested during an IVF treatment, they have actually been spared from atresia that would have occurred during that menstrual cycle.
It is also important to note, that whether or not they undergo IVF, women who struggle with infertility are usually already at risk of having poor ovarian reserve and reaching early menopause. One of the tests that can be used to detect low ovarian reserve is the Anti-Mullerian Hormone (AMH) blood test. Egg reserves and AMH levels usually decline with age and can be affected by environmental factors such as cancer treatment or ovarian surgery, as well as inherited genetic causes, endometriosis, tumors, immunological conditions and high body mass index.
With that in mind, studies conducted by research teams around the world, including the British Fertility Society, Queensland University, Australia, and Cornell University, US have confirmed that IVF, even with multiple cycles, does not lead to egg depletion nor early menopause.
Having studied hundreds of IVF patients through the years, these researchers have concluded that IVF does not affect the timing or severity of menopause symptoms. In fact, many IVF patients reach menopause at the average age of just over 50, which is comparable to most national averages and closely resemble that of their own mothers’. The studies also found that most respondents had given birth to at least one child as a result of IVF.
Dr Helena Spoke against Child Marriage & Advocated for Women’s Right on TV2, ‘What Say You Programme’


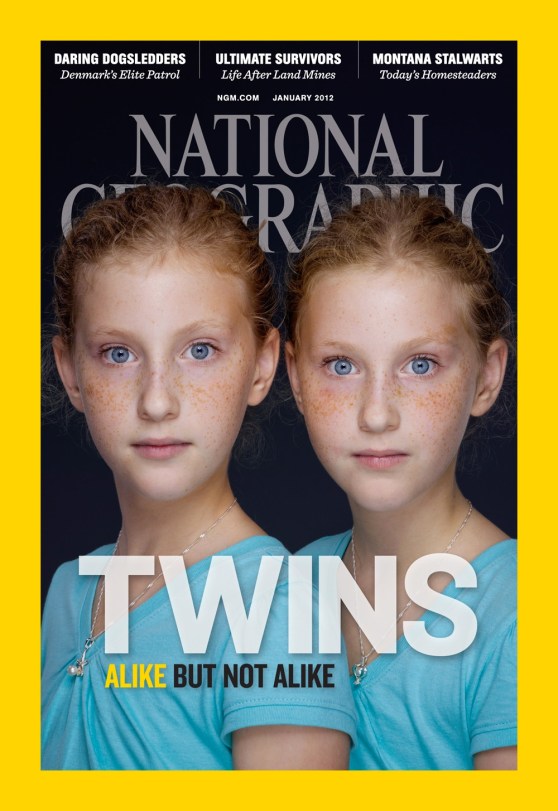
The occurrence of identical twins after a single embryo transfer
Even after many years of being a doctor, it still brings me immense joy to announce to my patient that she is indeed pregnant following a successful infertility treatment. And sometimes, the happiness is multiplied, as there isn’t one, but two buns in the oven!
In general, it is widely known that the occurrence of multiple births is much higher following assisted reproductive technologies (ART) as compared to incidences of twins in natural or spontaneous pregnancies. This is directly related to the number of embryos transferred back to the uterus. In general, if 2 embryos are transferred back into the uterus, the chance of having twin pregnancies is around 20-30%. As we all know, twin pregnancies carries more risks to the expecting mother as well as the babies. The risks of miscarriage, bleeding in pregnancy, high blood pressure, diabetes in pregnancy, Placenta Praevias, Caesarean Sections are some of the significant obstetric risks. The babies are also at risk of preterm births, stillbirths and complications associated with preterm deliveries such as cerebral palsies.
Therefore, in many countries especially in the west, it is mandatory that the patients are informed of these risks before an embryo transfer. Some countries had restricted the number of embryos transferred to one. This move had significantly reduce the incidence of twins following an IVF and had reduced the economic burden associated with medical care of pregnancies associated with twins

However, in recent years, it had been reported that there is a higher incidence of identical twins following single embryo transfer.
While the incidence of fraternal twins following the transfer of two embryos is an easily understandable consequence of IVF, the causes for identical twins after ART remain speculative at best. However, there is some evidence that attributes the phenomenon to the micromanipulation techniques, length of culture and culture medium used during treatment, as well as the genetics of the parents.
Identical twins, also known as monozygotic twinning or MZT, occur when an egg and a sperm unite to form a single zygote that divides into two embryos or separate individuals. It is a rare phenomenon, which occurs in only about 1% of natural conceptions. However, in assisted conceptions, the occurrence of monozygotic twinning almost doubles.
The splitting of the zygote into separate embryos can occur at any time during the first 2 weeks after fertilisation. However, the timing of the split will influence the type of identical twin. For example, in around 1/3 of MZT cases where the split occurs within 72 hours of fertilisation, the result is two placentas and two amniotic sacs. In the remaining 2/3 of MZT cases, the splitting occurs 4-8 days after fertilisation, resulting in one placenta and two amniotic sacs. And in about 5% of MZT cases, where splitting occurs 8-13 days after fertilisation, the outcome is one placenta and one amniotic sac. In very rare cases, the outcome is conjoined twins.
Although the prospect of having twins is certainly exciting, couples must also understand that twin pregnancies are considered high risk. They can lead to various pregnancy complications with long-lasting and even permanent effects for the children. These include caesarean section, premature birth, low birth weight, Twin-Twin Transfusion Syndrome (TTTS), pre-eclampsia, gestational diabetes, fetal abnormalities and congenital abnomalies. In view of the complications that can arise from a twin pregnancy, do speak to your infertility consultant about the risks involved should you have any worries.

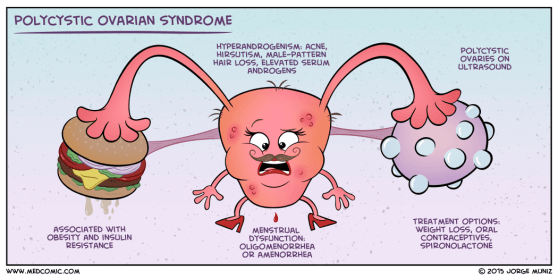
PCOS – What you should know
As a fertility doctor, I see women who are troubled by Polycystic ovary syndrome (PCOS) on a daily basis. Most of them come to see me because they have difficulty in trying to conceive and some of them have irregular menses, but many of them are unaware of their condition. Polycystic ovary syndrome (PCOS) is a relatively common health problem, affecting an estimated 1 out of 10 women of childbearing age. However, many women who come to see me are either unaware or misinformed about PCOS. To help dispel some of the misconceptions about PCOS, in today’s blog I’ll be explaining what PCOS is, what causes it and how it can be treated.
What is PCOS?
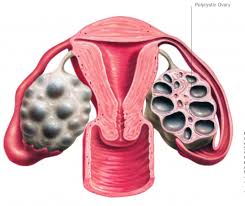
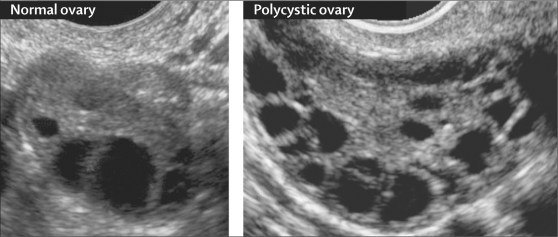
PCOS is a condition whereby small ‘cysts’ develop on a woman’s ovaries. In actual fact, these ‘cysts’ are not actually cysts per se, but are ovarian follicles which contain eggs. A healthy young woman will usually have about 5-10 follicles in each ovary, however, in the case of PCOS, each of the ovaries contain more than 10-12 follicles. Although these follicles are a sign of abundance in egg numbers, they cause the body to have hormone imbalances. Because hormones are chemical messengers, responsible for triggering various different processes in our bodies, when a hormone imbalance occurs it causes detrimental chain reactions.
For example, PCOS can cause the ovaries to produce more androgens (male sex hormones), which disrupts ovulation, causes irregular periods, as well as causes acne and extra body or facial hair. PCOS can also cause insulin resistance, which increases blood sugar levels and can cause diabetes over time.
Other health issues caused by PCOS are metabolism problems, heart disease and infertility. If you have a family history of PCOS, on either your mother or father’s side, your chance of getting it is much higher.
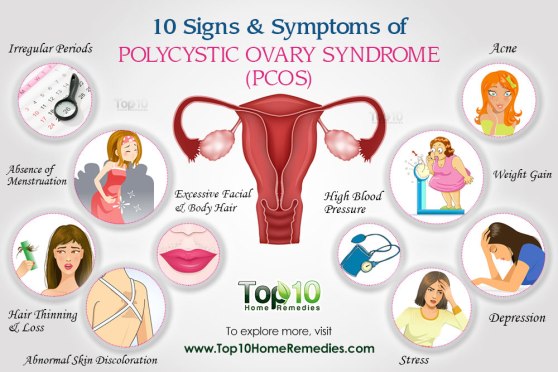
PCOS Symptoms
Most women with PCOS share a number of common symptoms such as weight gain or trouble losing weight; extra facial or body hair (especially on the face, chest, belly and back); hair thinning on the scalp; irregular, few or no periods; heavy periods; fertility problems and depression. You may have many or just a few of these symptoms.
Diagnosis
In order to diagnose PCOS, your doctor will begin by asking you a series of questions about your health, symptoms and menstrual cycles. This will be followed by a physical exam, which will look for excessive body hair and high blood pressure, as well as take note of your body mass index (BMI). Next, some of your blood will be drawn to test your blood sugar, insulin and other hormone levels. Finally, you may have a pelvic ultrasound to look for cysts on your ovaries. Early diagnosis and treatment is crucial, as it can help you to control the unpleasant symptoms of PCOS, as well as prevent long-term health problems.
Treatment
Positive lifestyle changes can have a profound effect in treating PCOS. They not only reduce the unpleasant symptoms that you may experience, but also help prevent long-term health issues. To kick start your PCOS treatment, fit in moderate to vigorous exercises to your daily routine, such as walking, swimming, aerobic dancing and bicycling.
You should also eat a healthier diet, comprising of lots of vegetables, fruits, nuts, beans and whole grains. You should also reduce your intake of high calorie food which are high in saturated fat and carbohydrate. These life style changes will improve your weight and reduces insulin resistance. If you are a smoker, quite smoking as it causes you to have higher androgen levels. Most polycystic women will also benefit from weight loss, which can help balance out your hormones and regulate your ovulation and menstrual cycle.
In addition to lifestyle changes, your doctor may prescribe you with medication to help reduce any symptoms you might be suffering, as well as to help you get pregnant. The common medications are ovulation inductions drugs, such as Clomiphene Citrate (Clomid) or FSH hormones injections. This will help you to ovulate naturally and increase your chance of pregnancy. Your doctor may also prescribe Metformin, which is a medication to reduce insulin resistance. This in turn will help to reduce weight, increase natural ovulations and reduces the androgenic effects of PCOS.
Laparoscopic ovarian drilling was once a popular surgery in reducing the effect of high androgens in PCOS patients. However, recent studies revealed that the effect of laparoscopic ovarian drilling is short-lived, i.e. the menstrual irregularity returns after a few months. On top of that, laparoscopic ovarian drillings has other adverse effects on women’s fertility, such as premature ovarian failure, adhesion formations causing tubal obstructions etc. Laparoscopic ovarian drilling is invasive and expensive especially in private settings. Therefore, it has become difficult to justify its cost against its effectiveness.

In some women, whereby there are other associated problems such as tubal obstructions or husbands’ sperms are weak or low in numbers, an IVF (In-vitro Fertilisation) treatment may be necessary and cost effective to achieve a pregnancy
Should you have any questions or concerns about PCOS and how it is affecting your health and chances of conceiving, as always, don’t hesitate to speak to your fertility consultant.
The loss of a pregnancy or miscarriage is something that most couples rather not think of. However, it’s important for couples to understand why miscarriages can happen, especially as it can be caused by various factors and steps can be taken to lower the risks. The common causes of miscarriage are anatomical causes (like uterine abnormality), genetic causes, immunological disorders and hormonal imbalance. In this article, I will address one of the most common types of hormonal imbalance known today – insulin resistance.
Insulin resistance is a condition whereby levels of sugar, estrogen and testosterone in the blood are raised, while progesterone levels are lowered. The result is an excess of glucose in the bloodstream, which leads to prediabetes, diabetes and other serious health disorders. In pregnancy, insulin resistance causes a variety of concerns, such as delayed fetal growth and gestational diabetes.
Several scientific studies have also found that insulin resistance can lead to miscarriage. One such study was carried out by a team of researchers at the Reproductive Medical Centre, Peking University, People’s Hospital, Beijing, China. After examining 107 patients that achieved their first pregnancy after infertility treatment, they came to the conclusion the risk of miscarriage can be directly linked to insulin resistance.
A team from the Obstruction & Gynecology Department, Babol University of Medical Science, Babol, Iran offered similar findings, when they proved that women with elevated insulin levels are at a higher miscarriage risk. As worrying as this is, it must be noted that insulin resistance doesn’t just heighten the risk of miscarriage; in fact, it has been shown to increase the risk of multiple miscarriages.
Several published studies have confirmed this, such as one by a team from the Department of Obstetrics and Gynecology at Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou. After investigating the differences in insulin resistance between women with recurrent miscarriage and those with normal pregnancy, they concluded that insulin resistance increases the risk for recurrent miscarriage during the first trimester of pregnancy.
The crucial link between insulin resistance and recurrent miscarriage was echoed in a prospective clinical study by a team of researchers from the Department of OB & GYN, Shiraz Medical University, Iran. Their study found that 39% of women with recurrent miscarriage have abnormal oral glucose tolerance test (OGTT) results. The OCTT, which measures the body’s ability to use glucose, is often used to check for insulin resistance and gestational diabetes.
Meanwhile, a team from the Division of Reproductive Endocrinology, Department of Obstetrics and Gynecology, University of Tennessee Health Science Center, Memphis, USA concluded that 27% of women with repeat miscarriage have high fasting insulin, despite normal glucose levels.
Insulin resistance is also associated with Polycystic Ovarian Syndrome or PCOS, which is why women with PCOS struggle with infertility. The condition raises levels of estrogen and testosterone in the body, while lowering progesterone levels. This interferes with the normal development of follicles in the ovaries, causing problems with ovulation.
However, if you have PCOS or insulin resistance and wish to undergo infertility treatment, hope is not lost. There are steps you can take to improve your insulin resistance sensitivity through lifestyle changes or medical intervention, before you undergo infertility treatment. Please don’t hesitate to speak to your infertility consultant should you have any concerns about insulin resistance. Your doctor can advise you on ways to reduce your risks and increase your chances for a safe pregnancy.


What do mental health, HIV, and erectile dysfunction have in common? These are just some well-known medical conditions that are still highly stigmatised. Why are some medical conditions stigmatised and how did some of them manage to break the stigma? Upper GI and Bariatric Surgeon Dr Reynu Rajan shares her experience dealing with bariatric patients in the face of weight-bias and discrimination, while Fertility Specialist Dr Helena Lim shares what it’s like to help patients overcome the taboo of infertility.
http://www.bfm.my/reynu-rajan-helena-lim-medical-conditions-stigma.html