Restoring balance
The benefits of acupuncture in IVF
In recent years, acupuncture has become an increasingly popular complementary treatment for those suffering from infertility, especially women undergoing IVF treatment. But what’s behind the buzz and does it actually work? Let’s examine the known facts.
What is acupuncture?
Acupuncture is a form of traditional Chinese medicine (TCM) and healing method that has been used for thousands of years across the world to treat a variety of ailments. It involves the gentle insertion of thin, sterile needles that are inserted into the skin at strategic points of the body to provide stimulation.
According to TCM practitioners, there are more than 2,000 acupuncture points on the human body, which are connect to 14 major pathways or meridians. These meridians conduct “qi,” which is a form of energy or life force that is believed to regulate our spiritual, emotional, mental and physical balance. Poor health habits can disrupt the proper flow of qi, leading to various ailments, including pain and infertility.

Benefits for those undergoing IVF
As acupuncture works on the principle of restoring balance, here’s how it can help:
Reduces stress – By lowering the levels of stress hormones released into the blood stream, acupuncture can help restore the body’s hormonal and neurochemical balance.
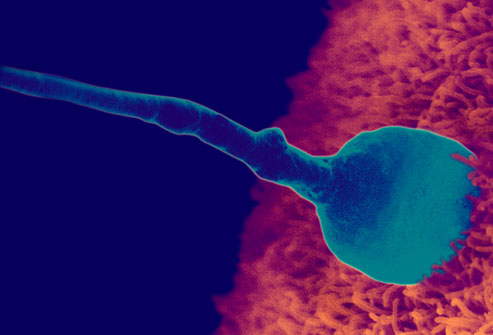
Improves blood flow – Stimulation at strategic points can increase blood flow to the ovaries and uterus, which increases chances for the egg to be implanted, nourished and carried to term.
Relieves aches – By alleviating existing aches and pains, acupuncture can provide further relief and stress reduction.
Relieves anxiety – By helping to treat conditions like anxiety and insomnia, which can have devastating long-term effects to wellbeing, acupuncture helps restore the body’s delicate balance.
Few side effects – Unlike some forms of Western treatment, which can be invasive and causes undesirable side effects, acupuncture has relatively few to no side effects other than causing bruising at the needle site.

Scientific research
Some experts in complementary medicine have cautioned that the positive effects of acupuncture may actually be due to a “placebo effect” that is caused by patients expecting acupuncture to work. To understand the phenomenon better, some scientific studies have been carried out to review the benefits of acupuncture in infertility treatments.
One study, jointly-conducted by the University of Maryland’s School of Medicine, Georgetown University School of Medicine, Washington and the University of Amsterdam, Holland, compared the results of needle acupuncture in women receiving IVF, against women who received fake treatments and no treatments at all.
The results were very positive, as according to the study, “IVF with acupuncture increased the odds of pregnancy by 65% (according to early evidence on ultrasound), increased the odds of ongoing pregnancy by 87% (according to ultrasound evidence of pregnancy at 12 weeks) and increased the odds of a live birth by 91% compared with IVF on its own.”

Conclusion
The researchers concluded that their results suggest that, “Acupuncture given with embryo transfer, improves rates of pregnancy and live birth in women who are undergoing in vitro fertilisation.” While their findings are significant and clinically relevant, the researchers consider them to be “somewhat preliminary” and call for further investigation in the link between pregnancy rates and the effect of acupuncture.
With these encouraging facts and figures, there is no wonder why more and more couples are choosing to include acupuncture in their infertility treatment routine. If you’re interested to find out more about using acupuncture as a complementary form of treatment, don’t hesitate to bring it up to your doctor.