Recently, a few patients came in with some information from the internet with regards to frozen embryos transfers. These information suggested that Frozen embryo transfers has a higher pregnancy rates compared to fresh embryo transfers. Therefore, the patients requested to undergo the IVF cycle so that they can freeze all the embryos and have the embryos transfer back in later cycles.
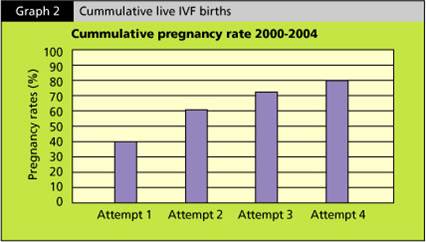
This practice is not something new. With the vast improvement in freezing technology using a new technique called ‘vitrification’ or rapid freezing method, the survival rates of embryos after freezing and thawing is close to 95%. Therefore, in a reasonably good IVF cycle, apart from having 2 embryos to transfer back during the fresh cycle, majority of patients would have good number of embryos to be frozen which can be used during the next cycle. It is not unusual to find that if the patients did not manage to get pregnant during the fresh cycle, when they come back for frozen embryo cycle, the pregnancy rates are close to 80-90%. A recent study conducted at KL Fertility Centre which looked at success rates of fresh cycles and frozen cycles of all women under the age of 42 and the statistic showed a 1.4x higher pregnancy rates for frozen embryos transfers. There is also significant lower miscarriage rate whereby there is a 2.5x reduction of miscarriage.
This finding coincides with the recent paper published in Fertility & Sterility, one of the world leading medical journal in Fertility. This paper consists of a meta analysis of a few studies which looked at the pregnancy rates for Fresh embryo transfers versus Frozen embryo transfers and the result showed a significant higher pregnancy rate in Frozen embryo transfers and a lower miscarriage rate. The results favoring Frozen Embryos Transfers instead of fresh embryo transfer may be related to the adverse effects of Controlled Ovarian Hyperstimulation (the drugs we used to stimulate your eggs to grow) on endometrial receptivity (which is the term we used for how ready your womb to accept the embryo for implantation) , as well as the improved results that can be achieved with current cryopreservation methods (which is the rapid freezing method, or vitrification). (Rogue M at el. Fresh embryo transfer versus frozen embryo transfer in in-vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013 Jan;99(1):156-62)
So, for those who have not been successful during the fresh cycle, please be reassured that when you come back for your frozen cycle, there is a higher chance of getting pregnant. Please do not beat yourselves up and turn the disappointment of the failed fresh cycle into a long-term grief. If you keep moving on, you will get there!!!!